Telehealth through the lens of value-based care in the US
By Xcenda
Updated: October 22, 2021
With the advance of technology and increasing needs of an aging population, telehealth has been playing an important role in transforming the delivery of healthcare. The ongoing coronavirus disease (COVID-19) pandemic and the expansion of value-based care (VBC) models have also contributed to its rapid adoption in the US. Telehealth can facilitate data-driven decision making and has great potential to assist providers, biopharmaceutical companies, and medical device manufacturers in reducing uncertainty in demonstrating the value of their products.
Trends of telehealth in the US
Telehealth is the use of medical information exchanged from one site to another through electronic communication to improve patient health. It is estimated that over 60% of healthcare institutions and around half of all hospitals in the US currently use some form of telehealth with four modalities implemented in patient care—live video (synchronous), store-and-forward (asynchronous), remote patient monitoring (RPM), and mobile health (mHealth).
The ongoing pandemic of COVID-19 has catalyzed the rapid adoption of telehealth and has changed the delivery of patient care in the US. It is reported that the proportion of visits using telehealth increased rapidly during the pandemic and over half (56%) of the behavioral health-related outpatient visits in December 2020 were virtual.
As the healthcare system in the US is transitioning from fee-for-service towards VBC models, telehealth provides special advantages in generating real-world evidence (RWE) that enable data-driven decision making, as well as improving patient outcomes and reducing healthcare resource utilization. Thus, telehealth will facilitate the adaptation to value-based purchasing (VBP) models and navigation of value-based agreements (VBAs) (Figure 1).
Figure 1. Use of telehealth in value-based care (VBC) models

Telehealth in VBC
Under VBC models, how to improve patient outcomes is a key consideration for many industry stakeholders. Telehealth has been shown to have numerous advantages in managing chronic diseases and improving physical and mental health, and supports the transition to VBC for health providers, biopharmaceutical companies, and medical device manufacturers.
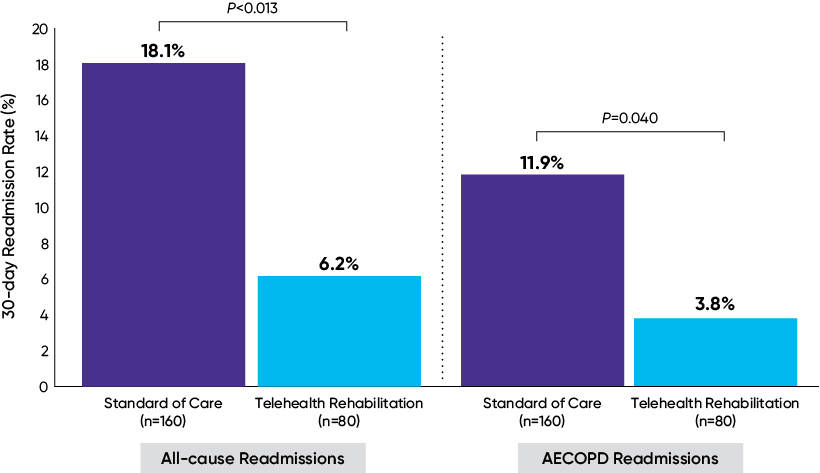
For example, telehealth can reduce hospital readmissions through better prevention, more timely intervention, and improved patient education and engagement. It has been proven that telehealth reduces the readmission rate in elderly patients with chronic obstructive pulmonary disease (COPD) or heart failure (HF) (Figure 2). Additionally, the use of telehealth has also been shown to reduce unscheduled in-clinic postoperative visits and result in higher patient satisfaction rates among patients who underwent elective primary total hip arthroplasty (THA) and total knee arthroplasty (TKA). These features of telehealth are in line with the goal of the Medicare Hospital Readmissions Reduction Program, which is a VBP model aimed at reducing 30-day risk-standardized unplanned readmissions among patients with acute myocardial infarction, COPD, HF, pneumonia, coronary artery bypass draft surgery, and THA and/or TKA. Besides Medicare, other state-level programs such as the Michigan Arthroplasty Registry Collaborative Quality Initiative also focuses on post-operative readmission reduction as an objective in their metrics. Thus, the appropriate use of telehealth can assist providers in their successful participation in such programs which provide incentive payments for quality of care.
Figure 2. Comparison of 30-day readmission rates between standard of care and telehealth rehabilitation for all-causes and for acute exacerbation of chronic obstructive pulmonary disease (AECOPD)
In addition, the VBP agreement between Allina Health and Blue Cross and Blue Shield of Minnesota lists the expansion of telehealth as one of the main focuses, aiming to provide care at the right time and place.
For companies offering telehealth technologies, the incorporation of the evidence requirements of these VBP programs, such as reduced hospital readmission, is encouraged early on in the product development process. This way findings that are relevant to providers’ financial objectives can be presented to decision makers at launch to shorten time to market. Focusing on tracking and improving patient’s interaction with and adherence to the prescribed telehealth technology is recommended to ease potential concerns about translating benefits from a controlled trial environment to the real world.
Telehealth in data-driven decision making
The transition of reimbursement and payment in the healthcare system from volume to value requires better capability in collection and evaluation of patient outcomes. To this end, RPM and mHealth could be used to generate rich RWE by enabling the collection and transmission of patient-reported outcomes and vital signs, such as blood glucose level, blood pressure, blood oxygen level, and heart rate, through mobile applications and wearable sensors. Although efforts are warranted to ensure user privacy and data security, with mHealth bridged into RPM, data analysis and patient engagement and education are available for better patient care and real-world research.
In the Prediction, Risk, and Evaluation of Major Adverse Cardiac Events (PRE-MACE) study, for example, consumer-grade biosensors were used to collect active and resting heart rate and electrocardiogram information, and a simple finger prick blood sample collection tool was used for remote collection of biochemical biomarkers, which allowed the analysis of blood protein composition, intermediate biomarkers, and lipid levels. Through a smartphone application, patient-provider communication was conducted based on the results of data-driven machine learning algorithms and patient-reported outcomes. Through the use of RPM, mHealth, and artificial intelligence, the PRE-MACE study was designed to examine the predictive validity for MACE among patients with ischemic heart disease and estimate the cost-effectiveness of RPM. This study will serve as a model for population-based telehealth in other chronic diseases as well. The appropriate use of telehealth in real-world data collection and analysis has great potential to facilitate evidence-based decision making focusing on quality of care and ensuring the right patients get the right treatment at the right time.
With the development of connected and personalized care, RPM and mHealth have demonstrated a great potential in consistent monitoring and collection of patient status, which leads to improved patient adherence and outcomes and enhanced RWE to facilitate VBA negotiation. This will allow timely confirmation of treatment efficacy to reduce uncertainty for all stakeholders. For example, through diabetes connected care, telehealth can facilitate the collection of credible A1c data among patients with diabetes beyond the traditional office visits setting or the less reliable patient self-report data.
Conclusion
As the US healthcare system transitions from fee-for-service to pay-for-performance models, telehealth is playing an increasingly important role in transforming the delivery of healthcare. It can facilitate and enhance VBC by improving patient outcomes, reducing healthcare resource use, and generating RWE. Given these advantages, the adoption of telehealth will benefit providers under VBP and result in an acceleration in its adoption. For biopharmaceutical companies and medical device manufacturers, telehealth can be utilized to improve patient outcomes and generate RWE to support VBA negotiation.
The article should be referenced as follows:
Zhang Q, Su W. Telehealth through the lens of value-based care in the US. HTA Quarterly. Winter 2021. https://www.xcenda.com/insights/htaq-winter-2021-telehealth-value-based-care-US/
Sources
- Andrès E, Meyer L, Zulfiqar AA, et al. Telemonitoring in diabetes: evolution of concepts and technologies, with a focus on results of the more recent studies. J Med Life. 2019;12(3):203.
- Bhatt SP, Patel SB, Anderson EM, et al. Video telehealth pulmonary rehabilitation intervention in chronic obstructive pulmonary disease reduces 30-day readmissions. Am J Respir Crit Care Med. 2019;200(4):511-513.
- Bhatt SP, Sanders JG, Anderson EM, et al. Telehealth exercise intervention reduces COPD readmissions. Am J Respir Crit Care Med. 2018;197:A4545.
- Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). August 6, 2021. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
- Eli Lilly and Company. Welldoc and Lilly collaborate to integrate BlueStar® app capabilities into Lilly's connected insulin solutions. February 25, 2021. https://investor.lilly.com/node/44686/pdf
- Fendrick AM & Chernew ME. Outcomes-based agreements give new insight for treatment of diabetes and cardiovascular disease. Profiles in Care. AM J Manag Care. August 2021.
- Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D, Schneider E. The impact of COVID-19 on outpatient visits in 2020: visits remained stable, despite a late surge in cases. Accessed October 19, 2021. https://www.commonwealthfund.org/publications/2021/feb/impact-covid-19-outpatient-visits-2020-visits-stable-despite-late-surge
- O’Connor M, Asdornwised U, Dempsey ML, et al. Using telehealth to reduce all-cause 30-day hospital readmissions among heart failure patients receiving skilled home health services. Appl Clin Inform. 2016;7(02):238-247.
- Office of Health Policy, Office of the Assistant Secretary for Planning and Evaluation. Report to Congress: E-health and telemedicine. Washington, DC: Department of Health and Human Services, August 12, 2016. https://aspe.hhs.gov/sites/default/files/pdf/206751/TelemedicineE-HealthReport.pdf
- Sharareh B & Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty. 2014;29(5):918-922.
- Shufelt C, Dzubur E, Joung S, et al. A protocol integrating remote patient monitoring patient reported outcomes and cardiovascular biomarkers. NPJ Digit Med. 2019;2(1):1-6.
- Thomason TR, Hawkins SY, Perkins KE, Hamilton E, Nelson B. Home telehealth and hospital readmissions: a retrospective OASIS-C data analysis. Home Healthc Now. 2015;33(1):20-26.
- Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585-1592.
Subscribe to HTA Quarterly



